new posts in all blogs
Viewing: Blog Posts Tagged with: hospital, Most Recent at Top [Help]
Results 1 - 17 of 17
How to use this Page
You are viewing the most recent posts tagged with the words: hospital in the JacketFlap blog reader. What is a tag? Think of a tag as a keyword or category label. Tags can both help you find posts on JacketFlap.com as well as provide an easy way for you to "remember" and classify posts for later recall. Try adding a tag yourself by clicking "Add a tag" below a post's header. Scroll down through the list of Recent Posts in the left column and click on a post title that sounds interesting. You can view all posts from a specific blog by clicking the Blog name in the right column, or you can click a 'More Posts from this Blog' link in any individual post.

By: Chloe Miller,
on 10/7/2016
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
Journals,
hospital,
Plastic Surgery,
OR,
medical insurance,
*Featured,
oxford journals,
Science & Medicine,
Health & Medicine,
patient safety,
aesthetic surgery,
aesthetic surgery journal,
surgical procedure,
ambulatory surgery center,
CosmetAssure,
elective surgery,
James C. Grotting,
office-based surgery,
office-based surgical facilities,
operating room,
patient health,
surgical safety,
Add a tag
Like many plastic surgeons, and as my aesthetic practice has grown, I prefer to perform most surgeries in my accredited, office-based operating room. By operating in my office, I have access to my own highly qualified team members who are accustomed to working together. In this way, we can create an experience for the patient that is more private, safe, efficient, cost-effective, and highly likely to produce optimal results.
The post How safe are office-based surgical facilities? appeared first on OUPblog.

By: Amy Walker,
on 9/23/2016
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
job satisfaction,
cardiology,
european heart journal,
european society of cardiology,
ESC,
Oxford Medical Handbooks,
Ellie Gregory,
esc congress,
healthcare workers,
Books,
inspiration,
Journals,
hospital,
Rome,
*Featured,
Science & Medicine,
Health & Medicine,
Online products,
Oxford Medicine Online,
Add a tag
The ability to improve the health of another person or to save their life requires great skill, knowledge, and dedication. The impact that this work has goes above and beyond your average career, extending to the families and friends of patients. We were interested to discover what motivates the people who play a vital role in the health and quality of life of hundreds of people every year.
The post What inspires the people who save lives? appeared first on OUPblog.

By:
Monica Gupta,
on 8/16/2016
Blog:
Monica Gupta
(
Login to Add to MyJacketFlap)
JacketFlap tags:
Chinese Manjha,
fallen through the roof,
injured bird,
interrupted electricity,
Sikar News,
Articles,
hospital,
kite flying,
Jaipur,
शौक,
पतंग,
Add a tag
आता माझी सटकली आता माझा सटकल लिया रे .. मांझे ने जान ली जानलेवा है ये शौक !! हादसे !! शौक बनाम शोक कल शाम मार्किट जाते वक्त अचानक हमने अपनी कार की स्पीड तेज कर् दी. भारी रश होते हुए भी हमे अपनी कार तेज इसलिए चलानी पडी क्योकि आगे एक महिला स्कूटर पर […]
The post आता माझी सटकली appeared first on Monica Gupta.

By: Amelia Carruthers,
on 2/5/2016
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
Science & Medicine,
Health & Medicine,
dialysis,
Kidney disease,
medical history,
Books,
Crafoord Foundation,
David Goldsmith,
Dialysis Machine,
Fourth Edition,
Gambro,
Nils Alwall,
Oxford Textbook of Clinical Nephrology,
Willem Kolff,
WWII,
Technology,
hospital,
machine,
Sweden,
surgery,
discovery,
World War Two,
*Featured,
Add a tag
During the night, between 3rd and 4th September 1946, things were stirring in the basement of the internal medicine department, at the university hospital of Lund, Southern Sweden. A 47-year-old man had been admitted for treatment. His main problem was uraemia (urea in the blood), but he was also suffering from silicosis (a lung disorder), complicated by pneumonia.
The post Nils Alwall: The quiet, unassuming Swede appeared first on OUPblog.

By: Amelia Carruthers,
on 11/6/2015
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
Health & Medicine,
Alan Glasper,
Charles West,
Childrens Healthcare,
Childrens Hospital Movement,
Childrens Nursing,
Great Ormond Street,
Oxford Handbook of Children's and Young People's Nursing,
Books,
History,
hospital,
Victorian,
British,
charles dickens,
nursing,
healthcare,
Pediatrics,
queen victoria,
florence nightingale,
*Featured,
Add a tag
At the dawn of the children’s hospital movement in Europe and the West (best epitomised and exemplified by the opening of London’s Great Ormond Street Hospital for Sick Children (GOSH) on 14 February 1852), the plight of sick children was precarious at all levels of society. After a long campaign by Dr Charles West, Great Ormond Street hospital was the first establishment to provide in-patient beds specifically for children in England.
The post Charles West and Florence Nightingale: Children’s healthcare in context appeared first on OUPblog.
I can honestly say, these past three months have been the most exhausting, frustrating, rewarding and fulfilling months in my life. Well, maybe not my life, but they certainly rank in the top five.
1. We moved offices.
It was a confusing, whirlwind mass of chaotic activity. We all knew we were going to move to our new office at the hospital, it was inevitable, but we were told it wouldn’t be until closer to Thanksgiving, so though we knew we were moving, we weren’t really PSYCHED to move. Suddenly, our new office was done and the CEO of the company didn’t see the need to delay the inevitable so we got the green light to move.
It wasn’t a slow, organized move, it was a crazy, throw everything in boxes and load up our cars move.
We moved on a Friday but we didn’t close up shop to move. It was business as usual and we packed our crap up in between patient phone calls. Each team was allotted about two hours to pack our crap, load it up and drop it off at the new office. Then, once the phones shut off at 4:30, we all went into frenzy mode and moved the rest of our stuff. We unloaded just the stuff we knew we would need for clinic on Monday and the rest stayed in boxes.
It was a crazy, disorganized but sort of fun time. And we survived our first clinic in our new place. My doctor was pretty patient, (what choice did he have?) and when we explained the situation to the patients, they were pretty understanding and patient, too. (Again, what choice did they have?)
I love this office. I truly do. It’s spacious and still has that NEW smell. We’re located on the 7th floor and we have a spectacular view of the city. We are the only specialty on our floor so we have the place to ourselves. I’m proud to work here. I know it’s impressive and people are impressed when they get to us.
We’ve had issues. We’ve had doors that wouldn’t open and doors that opened so fast that they were seriously a hazard to anyone within slapping distance. We have been unable to locate light switches and we still have problems with light-motion sensors that are too sensitive and often shut off leaving us in the dark and either having to wave our arms to bring the lights back on or we have to work in the dark until we physically get up to turn the damn things on again.
The toilets flush so loudly they are seriously damaging our eardrums and everyone has to hold their ears when they go off to protect ourselves. At least we won’t have to worry overly much about clogging them as I’m pretty sure they have so much suction they would suck a small child down the pipes if given the chance.
Our docs don’t have offices. Instead, we have collaboration spaces within each “pod.” We have five pods total. In fact, I’m using a collaboration space right now to write this. (More on that later). These collab spaces are intended to allow the physicians to sort of disappear whenever they need a break or want someplace private to eat their lunch. These collab spaces also double as meeting rooms or in my case, study spaces. Since the doctors are only in the clinic two times a week, they are in surgery the rest of the week, they didn’t see the need to have permanent spaces for temporary occupancy.
We’ve been in our space now for three months. Three months, in some ways, it feels a lot longer. We still don’t have enough stools to sit on in the exam rooms and supplies to supply 55 exam rooms. (Each pod has five exam rooms each – we also have one large procedure room in case the doctors need to treat wounds or more complicated issues). For several weeks, we didn’t have enough scales and we had to routinely share and move scales around in order to work our clinics.
Even though we are the only specialty on our floor, we still have room to grow. The front part of our floor is undeveloped and locked off. I have no idea what the hospital plans on doing with this undeveloped space and can only guess that it’s intended to add on more doctors, but we’ll see. So that’s exciting, knowing that at some point, there are likely more changes in our future.
If you can count on anything in business, it’s change.
Let me see if I can explain this set up for you …
When you get off the elevators, you can only go one way and that way is to a centralized podium. The person at the podium then “blues” you in on the schedule so that people like me will know you’re on the floor. The podium person will then direct you to the pod where your doctor is located. I work out of pod 5. Patients will then settle into our waiting room and wait for me to call them back to a room where I start their charts and get their vitals.
On Wednesdays, we share the waiting room with another doctor and last week it was so crowded it was literally standing room only. It’s so weird how the patient flow works out – we will be an hour ahead of schedule and suddenly, we have an influx of patients and we’re an hour behind.
I think this week, I’m going to ask my doctor if he would mind if we used the main waiting area – the area that people see when they first get off the elevators. It’s just too confusing for patients and awkward for me to try and keep track of everyone.
I’m all about efficiency. In fact, I’ve sort of developed a reputation for being “on top of it.” I probably over plan clinics but in my mind, a little preparation goes A LONG WAY towards a more organized clinic. In fact, I’m pretty sure my doctor has come to expect this preparation from me now so there is no way I would NOT plan my clinics, I wouldn’t want to disappoint him.
Which leads me to the second big work change ..
2. We finally switched over to the hospital charting software program in August.
The hospital has been “warning” us for years this change was going to happen so it’s not surprising that it happened once we moved onto the hospital campus.
We spent weeks staying after work transferring people over on to the new schedule program and into the new charting system. It was exhausting but it allowed us to make extra money and to familiarize ourselves with the new program so that ultimately, we taught ourselves how to get around it faster than if we hadn’t stayed to do data entry.
The first week we went live, we had software representatives available for questions. Which sounds awesome on the surface, but wasn’t really awesome in reality. Though they knew their way around the program, they were unfamiliar with our specialty and our specific needs. I can’t tell you the number of times I heard, “well, this is the way it’s supposed to work, but the feature is not working now.” After a time, they were just in the way and became super annoying to have around.
You could FEEL the tension emanating off our bodies that first week we went live. IT. WAS. FRUSTRATING. to say the least. And it’s still frustrating to this day. It’s hard to find anything, let alone quickly. Everything is filed into folders, each doc has a folder, I have a folder for all of the documents I put into the patient’s chart, every type of document has a folder, days have folders, it’s pretty insane, quite frankly.
And the programs, the charting program and the scheduling programs, are GLITCHY. Things will disappear, or we get error messages, or the program will just shut down. And our servers SUCK. They are SO SLOW. In fact, these programs are SO glitchy and slow that our ER finally put their foot down and refused to use it. They use something different.
It’s not unusual for me to completely shut down my computer, several times a day because it just locks up.
AARGH.
I think our docs had the most trouble with the program. They were definitely not set up the way our physicians wanted them to be set up and we’re constantly coming up with ways to get around restrictions. The hospital will likely figure out some of the workarounds we’re doing but that’s the only way our physicians can get their work done so I’m sure the hospital, at some point, will no choice but to make those changes. In the interim, we make do.
So. We moved on July 17th and went to a new software system one month later.
I was working 60 hour weeks for WEEKS during this process. I’m just NOW getting to a point where I’m now going home at 6:00 instead of 8:00. I haven’t seen my family in three months. Truly, I haven’t been home to have dinner with Kevin or the boys, during the week, in three months. I haven’t had time to stop. It’s been crazy.
Some of that crazy came from our phones.
3. We FINALLY went back to voicemails.
Some knucklehead had the bright idea that answering all of our calls live was the way to go. And for a while, it seemed to work. We answered live calls and did our best to help the patient with his/her questions/requests. But after a while, that’s ALL we did. Let me break it down for you.
Monday – I was in clinic. So I didn’t answer calls. I focused primarily on making sure the clinic ran smoothly.
Tuesday – I needed to schedule the Monday clinic patients for testing, but I didn’t have time to do that because I was in the pit answering live calls. So, I was taking calls for other doctor patients who had to tell their stories, from the beginning, to me because I was not familiar with their background. And then, being on a new system, it look three times as long to look anything up because we couldn’t find the damn information. AND/OR we had (still have to) access our old system – so in essence, we were working out of four systems, our old charting/scheduling programs and our new charting/scheduling programs. And when you answered live calls, you had to stop what you were doing before the call, to take the call, and when you hung up, you didn’t have time to start your own work because the damn phone would instantly ring.
Can you tell I LOATHE the phones??
Wednesday – I’m back in clinic. And I haven’t had a chance to touch my Monday clinic.
Thursday/Friday – I’m back on the damn phones. And again, I do not have a chance to get my clinic work done because I”m now forced to take care of patients for all of the docs. So the ONLY time I had a chance to clean up my week’s clinics AND prepare for my upcoming clinics, was after hours.
It was an insane process.
And to top it off, I started having chest pains. I don’t know if it was because I was under so much stress and working 60 hours weeks, or if it due to gas from starting to take Coconut supplements, or maybe a combination of both, but I ended up in the ER one night.
I was working clinic on a Wednesday and I just couldn’t breathe. I felt like I had to continuously take large breaths in order to function. I made several trips to the restroom just so I could pause, close my eyes and force my body to settle down. I took my blood pressure and it was way high. And my heart rate was over 100. I had chest pain but no arm/jaw pain so I really didn’t think I was having a heart attack but something was OFF.
Then that night, I just couldn’t sleep. My heart was racing double time and I was laying down!! I started hyperventilating and text Kevin (because he was at band practice) and he rushed home and took me to the ER. They hooked me up to an EKG machine and luckily, I wasn’t have a heart attack. They put me into a room and gave me liquid Ativan. Liquid GOLD, I say. That calmed me right down and my blood pressure went back down to normal. They didn’t give me an explanation for my crazy, but I’m pretty sure I had a panic attack. I think the pressure just got to me and I snapped.
I haven’t had an attack since then. I’ve adapted and learned to cope with this stress.
We had another person in the office break out into a rash because of the stress. When the director of our department found out about our physical manifestations to all of this stress, he put his foot down – it was time for changes.
We narrowed down that the phone situation just wasn’t working for us. So, we called our communications department in and they set it up so that each doctor has a voicemail now. Now, I can get to phones on MY time. And I’m already familiar with my doctor’s patients so that cuts down on response time. And I can return phone calls all at once so it’s way more efficient for everyone.
We’ve been back on voicemails for several weeks now and everyone is WAY more relaxed. We have time to BREATHE. We can all go to lunch together, if we want. We’re more in control of our processes and time. And that has left more time for me to pursue my next goal …
4. I’m studying for my CMA test
The CMA test is the Certified Medical Assistant test. The hospital has put together a pretty sweet incentive package for the medical assistants to become certified. It’s better for us, for the doctors and of course, for the hospital. So that has motivated all of us to study for the thing. A few of use have been staying late, or coming in on the weekend (like today – but I’m writing to you instead because I was feeling it today), to prepare for this. It costs $150 dollars to take the 3 hours test so I’m also motivated to take this pretty seriously because I don’t want to blow $150.
I’ve purchased study materials and I plan on purchasing a practice test so that I can focus my studies on the sections that will be on the test. I’ve only really been studying seriously for the past several weeks and I already feel like I’ve learned a lot. It’s stressful though – I feel like I’m cramming four years of medical school into about six weeks. I’m not going to tell you, or anyone I work with, the actual date I plan on taking this test, that way, if I fail, no harm, no foul. My goal is to just announce to everyone that I passed. If I told everyone my plans, took the test and then failed, I’m pretty sure I would be too mortified to show my face again. Everyone is wanting to go take it on the same day, but I simply can’t do that – I will be a bundle of nerves anyway, let alone taking the test with a bunch of people I work with.
The hospital is not only offering a bonus for becoming certified, but they’re also offering an hourly pay increase. And it’s a pretty sweet jump, let me tell ya.
So yes. I’m focusing my energies onto passing this thing now. I’ve been staying after work not only to finish my work, but on collaborating with my fellow co-workers on studying for the CMA.
I’m looking forward to the day when things get back to normal. Our entire worlds, and not just working worlds, but personal worlds, have been turned upside down these past several months.
But then I’ll have continuing education requirements after I pass the CMA in order to KEEP my CMA status.
It just never ends, does it.
Filed under:
Work Stuff 

By: Catherine Fehre,
on 1/2/2015
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
Books,
doctor,
hospital,
medical students,
primary care,
*Featured,
Science & Medicine,
Health & Medicine,
Kenneth M. Ludmerer,
Let Me Heal,
medical education,
residency training,
specialty medicine,
The Opportunity to Preserve Excellence in American Medicine,
Add a tag
The country has long had too many specialists and subspecialists, so the common wisdom holds. And, the common wisdom continues, the fault lies with the residency system, which overemphasizes specialty medicine and devalues primary care, in flagrant disregard of the nation’s needs.
It was not always that way. Before World War II, medical education practiced birth control with regard to the production of specialists. Roughly 80% of doctors were general practitioners, only 20% specialists. This was because the number of residency positions (which provided the path to specialization) was strictly limited. The overwhelming majority of medical graduates had to take rotating internships, which led to careers in general practice.
After World War II, the growth of specialty medicine could not be contained. The limit on residency positions was removed; residency positions became available to all who wanted them. Hospitals needed more and more residents, as specialty medicine grew and medical care became more technologically complex and scientifically sophisticated. Most medical students were drawn to the specialties, which they found more intellectually exciting and professionally fulfilling than general practice (which in the 1970s became called primary care). The satisfaction of feeling they were in command of their area of practice as an additional draw, as was greater social prestige and higher incomes. By 1960, over 80% of students were choosing careers in specialty medicine — a figure that has not changed through the present.
The transformation of residency training from a privilege to a right embodied the virtues of a democratic free enterprise system, where individuals were free to choose their own careers. In medicine, there were now no restrictions on professional opportunities. Individual hospitals and residency programs sought residents on the basis of their particular service needs and educational interests, while students sought the field that interested them the most. The result was that specialty and subspecialty medicine emerged triumphant, while primary care languished, even after the development of family practice residencies converted primary care into its own specialty.
This situation poses a perplexing dilemma for the residency system. More and more doubts have surfaced about whether graduate medical education is producing the types of doctors the country needed. No one doubts that having well-trained specialists is critically important to the nation’s welfare, but fear that graduate medical education has overshot the mark. Ironically, no one knows for sure what the proper mix of specialists and generalists should be. A popular consensus is a 50-50 mix, but that is purely a guess. One thing is clear, however: The sum of individual decisions is not meeting perceived public needs.
At the root of the problem is that fundamental American values conflict with each other. On the one hand, the ascendance of specialty practice service serves as a testimony to the power of American individualism and personal liberty. Hospitals and medical students make decisions on the basis of their own interests, desires, and preferences, not on the basis of national needs. The result is the proliferation of specialty practice to the detriment of primary care. This situation occurs only in the United States, for the rest of the Western world makes centralized decisions to match specialty training with perceived workforce needs. Medical students in other countries are not guaranteed residency positions in a specialty of their choice, or even a specialty residency in the first place.
On the other hand, by not producing the types of doctors the country is thought to need, there is growing concern that graduate medical education is not serving the national interests. This would be a problem for any profession, given the fact that a profession is accountable to the society that supports it and grants it autonomy for the conduct of its work. This poses an especially thorny dilemma for medicine, in view of the large amounts of public money graduate medical education receives. Some medical educators worry that if the profession itself cannot achieve a specialty mix more satisfactory to the public, others will do it for them. Various strategies have been tried — for instance, loan forgiveness or higher compensation for those willing to work in primary care. However, none of these strategies have succeeded — in part because of the professional lure of the specialties, and because of the traditional American reluctance to restrict an individual’s right to make his own career decisions. Thus, the dilemma continues.
Headline image credit: Hospital at Scutari, 1856. Public domain via Wikimedia Commons.
The post Residency training and specialty mis-match appeared first on OUPblog.


By: Julia Callaway,
on 11/7/2014
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
Books,
hospital,
*Featured,
Science & Medicine,
Health & Medicine,
working hours,
Kenneth M. Ludmerer,
Let Me Heal,
Medical Residency,
ACGME,
house officers,
Libby Zion,
medical student,
Add a tag
Interns and residents have always worked long hours in hospitals, and there has always been much to admire about this. Beyond the educational benefits that accrue from observing the natural history of disease and therapy, long hours help instill a sense of commitment to the patient. House officers learn that becoming a doctor means learning to meet the needs of others. This message has never been lost on them.
However, it has also long been recognized that house officers are routinely overworked. This point was emphasized in the first systematic study of graduate medical education, published in 1940. In the 1950s and 1960s, the hazards of sleep deprivation became known, including mood changes, depression, impaired cognition, diminished psychomotor functioning, difficulty with interpersonal relationships, and an increased risk of driving accidents. In the 1970s, the phenomenon of burnout was recognized. In the mid-1980s, after prospective payment of hospitals was introduced, the workload of house officers became greater still, as there were now many more patients to see, the patients were sicker, the level of care was more complex, and there was less time with which to care for patients. House officers understood they were in a dilemma where their high standards of professionalism were used by others to justify sometimes inhumane levels of work.
Despite their long hours, the public generally believed that house officers provided outstanding medical and surgical care. Through the 1980s, the traditional view that medical education enhanced patient care remained intact. So did the long-standing belief that teaching hospitals provided the best patient care — in large part because they were teaching hospitals.
In 1984, the traditional belief that medical education leads to better patient care received a sharp rebuke after 18-year old Libby Zion died at the New York Hospital. Ms. Zion, a college freshman, had presented to the hospital with several days of a fever and an earache. The next morning she was dead. The case quickly became the center of intense media interest and a cause célèbre for limiting house officer work hours.
The public’s fear about the safety of hospitals increased in the 1990s. In 1995, a seeming epidemic of errors, including wrong-site surgery and medication and medication mistakes, erupted at US hospitals. These high-profile tragedies received an enormous amount of media attention. The most highly publicized incident involved the death of 39 year-old Betsy Lehman, a health columnist at the Boston Globe, from a massive chemotherapy overdose while being treated for breast cancer at the renowned Dana-Farber Cancer Institute. Public concern for patient safety reached a crescendo in 1999, following the release of the Institute of Medicine’s highly publicized report To Err Is Human. The report concluded that 48,000 to 98,000 Americans died in US hospitals every year because of preventable medical errors.
The result was that in the early 2000s, a contentious debate concerning resident work hours erupted. Many within the medical profession felt that work-hour regulations need not be imposed. They correctly pointed out that little evidence existed that patients had actually suffered at the hands of overly tired residents, and they also claimed that resident education would suffer if held hostage to a time clock. Critics, particularly from outside the profession, pointed to valid physiological evidence that fatigue causes deterioration of high-level functioning; they also argued that high-quality education cannot occur when residents are too tired to absorb the lessons being taught. As the debate proceeded, the public’s voice could not be ignored, for the voices of consumer groups and unions were strong, and Congress threatened legislative action if the profession did not respond on its own
Ultimately, the medical profession acquiesced. In 2002, the Accreditation Council for Graduate Medical Education (ACGME), which oversees and regulates residency programs, established new work-hour standards for residency programs in all specialties. Effective 1 July 2003, residents were not to be scheduled for more than 80 hours of duty per week, averaged over a four-week period. Over-night call was limited to no more frequently than every third night, and residents were required to have one day off per week. House officers were permitted to remain in the hospital for no more than six hours after a night on-call to complete patient care, and a required 10-hour rest period between duty periods was established.
Ironically, as the ACGME passed its new rules, there was little evidence that resident fatigue posed a danger to patients. The Libby Zion case, which fueled the public’s concern with resident work hours, was widely misunderstood. The problems in Ms. Zion’s care resulted from inadequate supervision, not house officer fatigue. At the time the ACGME established its new rules, the pioneering safety expert David Gaba wrote, “Despite many anecdotes about errors that were attributed to fatigue, no study has proved that fatigue on the part of health care personnel causes errs that harm patients.”
On the other hand, the controversy over work hours illustrated a fundamental feature of America’s evolving health care system: Societal forces were more powerful than professional wishes. The bureaucracy in medical education responded slow to the public’s concerns that the long work hours of residents would endanger patient safety. Accordingly, the initiative for reform shifted to forces outside of medicine — consumers, the federal government, labor, and unions. It became clear that a profession that ignored the public’s demand for transparency and accountability did so at its own risk.
The post The origin of work-hour regulations for house officers appeared first on OUPblog.


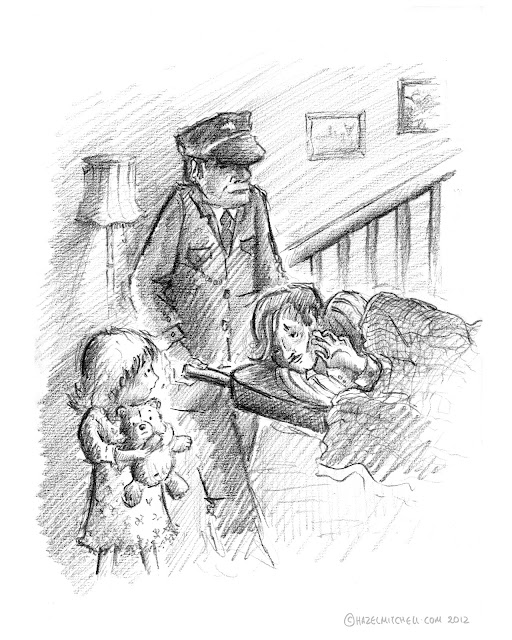
By: Hazel Mitchell,
on 7/18/2012
Blog:
Hazel Mitchell
(
Login to Add to MyJacketFlap)
JacketFlap tags:
illustration,
children's illustration,
hospital,
childhood,
illness,
childhood memories,
Hazel Mitchell,
sketch for today,
look back in candour,
Add a tag
Remembering is hard ... especially from younger years. Are the memories from photographs, from tales told to you later in life? Or real snapshots in your mind? Perhaps it's a mixture of them all.
Having been in avoidance of diarying for many years my solution is to recall my memories as visuals.
I believe this will be a worthwhile journey, if difficult at times.
Toodles!
Hazel

By: Nicola,
on 1/26/2012
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
dementia,
delirium,
*Featured,
oxford journals,
age and ageing,
Science & Medicine,
Health & Medicine,
acute confusional state,
anayo akunne,
cognitive impairment,
health economics,
john young,
lakshmi murthy,
preventing delirium,
interventions,
impairment,
anayo,
akunne,
guideline,
multi,
health,
hospital,
NHS,
prevention,
elderly,
healthcare,
NICE,
Add a tag
By Anayo Akunne
Delirium is a common but serious condition that affects many older people admitted to hospital. It is characterised by disturbed consciousness and changes in cognitive function or perception that develop over a short period of time. This condition is sometimes called “acute confusional state.”
It is associated with poor outcomes. People with delirium have higher chances of developing new dementia, new admission to institutions, extended stays in the hospital, as well as higher risk of death. Delirium also increases the chances of hospital-acquired complications such as falls and pressure ulcers. Poor outcomes resulting from delirium will reduce the patient’s health-related quality of life but also increase the cost of health care.
Delirium can be prevented if dealt with urgently. Enhanced care systems based on multi-component prevention interventions are associated with the potential to prevent new cases of delirium in hospitals. Prevention in a hospital or long-term care setting will lead to the avoidance of costs resulting from patients’ care. For example, the cost of caring for a patient with severe long-term cognitive impairment is high, and prevention of delirium could reduce the number of patients with such impairment. It will therefore reduce the cost of caring for such patients. Prevention could reduce lost life years and loss in health-related quality of life due to other adverse health outcomes associated with delirium.
The multi-component prevention interventions involve making an assessment of people at risk in order to identify and then modify risk factors associated with delirium. Delirium risk factors targeted in such interventions normally include cognitive impairment, sleep deprivation, immobility, visual and hearing impairments, and dehydration. The people at risk of delirium have their risk of delirium reduced through such interventions. The implementation of these interventions is usually done by a trained multi-disciplinary team of health-care staff. This means additional implementation cost. It would therefore be useful to know if this set of prevention interventions would be cost-effective. It was indeed found to be convincingly cost-effective by the UK National Institute for Health and Clinical Excellence (NICE) and was recommended for use in medically ill people admitted to hospital.
It is cost-effective to target multi-component prevention interventions at elderly people at both intermediate and high risk for delirium. It is an attractive intervention to health-care systems. In the United Kingdom the savings for the intervention would spread unevenly between the National Health Service (NHS) and social care providers. The savings to the NHS may be modest and largely accrue through lower costs resulting from reduced hospital stay, whereas the savings to social care are likely to be more considerable resulting from an enduring and diminished burden of dependency and dementia, particularly reduced need for expensive care in long-term care settings. The NHS acute providers may need to invest to implement the intervention and to accrue savings to the wider public sector. The current NHS hospital funding system does not incentivise this type of investment, and this could be a major structural barrier to a widespread uptake of delirium prevention systems of care in the UK.
In the work undertaken as part of the NICE guideline on delirium, the additional cost of implementing the intervention was based on the description of the intervention that required additional staff for delivery. It is possible that the guideline provides an important under-estimate of cost-effectiveness. This is because it might be possible to implement the intervention within existing resources. The intervention is designed to address risk factors for delirium by delivering the sort of person-centred routine c

By:
admin,
on 7/11/2011
Blog:
Litland.com Reviews!
(
Login to Add to MyJacketFlap)
JacketFlap tags:
A Fairy Tale Retold,
authentic relationships,
dorms,
Regina Doman,
same sex attraction,
review,
ya,
teens,
book reviews,
books,
reading,
adventure,
book,
literature,
gay,
fiction,
fairy tale,
novel,
young adult,
ethics,
young adults,
fairy,
God,
teaching,
college,
Mystery,
character,
hospital,
teen,
depression,
therapy,
fire,
Christian,
healing,
abuse,
book club,
mental illness,
Sleeping Beauty,
freshman,
morals,
Catholic,
pro-life,
gender identity,
Briar Rose,
sexual assault,
nun,
vigil,
scholar,
Summer/vacation reading,
ethics/morality,
teachers/librarians,
Add a tag
 WAKING ROSE: A FAIRY TALE RETOLD
WAKING ROSE: A FAIRY TALE RETOLD
Doman, Regina. (2007) Waking Rose: a fairy tale retold. Front Royal, VA: Chesterton Press. ISBN #978-0-981-93184-5. Author recommended age: 16 +. Litland.com also recommends 16+. See author explanation for parents at http://www.fairytalenovels.com/page.cfm/cat/116//
Publisher’s description: Ever since he rescued her from Certain Death, Rose Brier has had a crush on Ben Denniston, otherwise known as Fish. But Fish, struggling with problems of his own, thinks that Rose should go looking elsewhere for a knight in shining armor. Trying to forget him, Rose goes to college, takes up with a sword-wielding band of brothers, and starts an investigation into her family’s past that proves increasingly mysterious. Then a tragic accident occurs, and Fish, assisted by Rose’s new friends, finds himself drawn into a search through a tangle of revenge and corruption that might be threatening Rose’s very life. The climax is a crucible of fear, fight, and fire that Fish must pass through to reach Rose and conquer his dragons.
Our thoughts:
It is difficult to capture the essence of this story coherently because it touches upon so many aspects of life. There is the mystery, of course, and continuing depth of family loyalty amongst the Briers. The craziness of those first years experienced when young adults leave their nest and venture into the outer world of college life, whether as newbie freshmen or advanced graduate students. Unlikely friendships as the strong nurture the weak with Kateri mentoring Donna in her mental illness, and Rose guiding Fish through abuse recovery. Fish’s loyalty to Rose, taken to the extreme, becomes unforgiving. But then self-denigration turns into enlightenment and hope.
And after all of that is said, we are left with the relationship of Fish and Rose finally reaching a neat and tidy conclusion :>)
The girls have progressed in the series to young adults. Blanche just married Bear and Rose is off to college. Fish continues in his college program too. Doman shows us the challenges young adults face when they first enter the world on their own, particularly in making friends and exploring crushes. We can imagine ourselves engaged in the chit chat and horseplay typical in budding relationships. Important also is the picture implanted in our mind of courtship.
Throughout the story, we can see the existence of three pillars: faith, family and friends. Whenever one of these pillars is weakened, internal conflict and unsafe situations arise. Maintaining the balance, we see Rose’s keen ability for discernment that has been honed as a result of consistency in faith life, family home “culture, and choice of friends. Her discernment is key to good decisions, keeping safe, etc.
Going beyond stereotypes, the dialogue paints a clear picture of the perceptions held by non-Christians against Christians, countered with a realistic portrayal of the passionate young Christian student. Previous books portrayed ac
My wiferecently had a successful back operation at Highland Hospital in Rochester. Shestayed on the sixth floor. Doctors and staff were great. And something else wasgreat: the view from her window. You could see downtown Rochester, including Kodak and other important buildings. We actuallysaw a fantastic sunset over Rochester #12 School. I always feel a nostalgic when I see an elementary school--that is, I wish that I was in it performing poetry.
I had no camera until the next day. So, I took this shot in the morning...
Not far from Mar's room there was a visitor's lounge where I took this photo through a smudged-caked window...
Home Sweet Home!

This illustration is from my early days as an illustrator. I did a lot of work for my client Cedars-Sinai Medical Center in those days and this is one of them for a cover of their in house magazine: LifeLines!
-Mike
Posted on 9/20/2009
Blog:
Time Machine, Three Trips: Where Would You Go?
(
Login to Add to MyJacketFlap)
JacketFlap tags:
UK,
Chocolate,
coffee,
Weird,
hospital,
Custard,
bizarre,
tea,
cream,
cookie,
British,
injury,
treat,
Offbeat,
biscuit,
Add a tag

Image via Wikipedia
Like many British people (and I suspect many other people around the world), it’s a real treat to crunch on a biscuit when enjoying a cup of tea or coffee. So you can imagine my surprise, when having my early Sunday morning imperfectly made cuppa (see http://purpleslinky.com/offbeat/the-complicated-cuppa-cup-that-cheers-or-mug-of-misery/) that I discovered I was amongst those idiots who have managed to suffer a minor injury at the hands of the humble hobnob.
http://www.express.co.uk/posts/view/125767/Crumbs-half-of-us-have-been-injured-by-biscuits
I regret to admit that I’m one of the 29% of adult Brits who have managed to splash themselves with hot tea when dunking my digestive. For those of you who’ve never dunked or heard of dunking let me enlighten you. Once you’ve made your tea (or coffee) (beverage) and taken the biscuit of your choice from the biscuit tin (dunkee), you then proceed to dip a bite size piece of the dunkee into the beverage while holding onto the remainder to use as a ‘handle’ . Once the dunkee has been dunked for a couple of seconds you bring it to the surface of the beverage and then manouevre the dunkee together with beverage as close to your chin as you can before biting (or sucking) the dunkee. The skill is in getting dunkee to lips before it drops back into the beverage. More often than not the dunkee drops its load back into the beverage thereby splashing the dunker with hot beverage!
If you’re lucky enough to dodge the hot beverage if the dunkee drops, don’t believe for one minute that the danger ends there. You then have the job of taking a teaspoon, delving to the bottom of the beverage and trawling the cup to retrieve the errant dunkee to prevent choking. This is no mean feat as, more often than not, the dunkee slips back into the beverage like an eel through a fishing net, which again can cause the dunker injury from splashback!
Having overcome the hazards of dunking, I have also regularly fallen into the 28% of Brits who have choked on biscuit crumbs and at times I’ve fallen into the 7% of Brits who have dropped a biscuit tin on their foot and the 7% who’ve been nibbled by a pet while feeding it with a biscuit (obviously I’m so sweet they can’t tell the difference between a biscuit and me), but thankfully none of my injuries have required the services of the A&E Department of the local hospital.
So there you have it – the Great British Biscuit Bite Back!! I’m now going to get my mid morning coffee and I’m just pondering on whether to risk having a Bourbon (the UK version of the Oreo) biscuit – could be a nice treat or could end up as ‘death by chocolate’!!! If it turns out to be the latter then at least I will have died happy!

You go to the hospital, lets say the emergency room they have you laying on a narrow bed, your barely dressed and afraid to move; and people are coming in and out like it is the local supermarket. You have the right for privacy and you should demand it.

Image via Wikipedia
The worst is when they are not too sure why your have hives and a fever, they seem to bring in several medical students and now they are discussing your situation. WHY!
After they leave the curtained area, you ask the person with you, or the nurse why is it necessary that so many people have to come parading around you. If told that this is a teaching hospital, inform them that you don’t recall signing anything that said you could be put on display. You want to be diagnosed, cured and sent home!
How about the pregnant woman, who goes into labor and constantly being checked on, by a different person every hour; or they look in through the little square glass window. Where is your right to privacy? The longer your labor the more faces you will see.
So the next time you find yourself staying in a hospital, let them know how you feel; it is your right to have privacy. It does not matter if you’re in the Emergency Room, Recovery Room, or you have been admitted and people just wonder in and out. If after speaking the staff, ask for a supervisor; and voice how you feel.
Some people are afraid to complain, but you should not; others will wait until they are home to complain, as not to be treated rudely during your stay. If it is your intention to file a complaint after you are discharged, make sure you take down names, along with the date and shift that they worked.
Service is very important, and if your feel that your personal privacy was invaded; you have the right to let the Board of Directors and supervisor know!

By: Rebecca,
on 8/13/2007
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
sick,
hospital,
clinical,
consultant,
Health,
Science,
A-Featured,
Medical Mondays,
dysmorphologist,
bedside,
reardon,
geneticist,
Add a tag

William Reardon, author of The Bedside Dysmorphologist: Classic Clinical Signs in Human Malformation Syndromes and their Diagnostic Significance, is Consultant Clinical Geneticist, at Our Lady’s Hospital for Sick Children, Crumlin, Dublin, Ireland. Dysmorphology is the study of congenital malformations. Often a health professional will take note of low set ears or deep set eyes and wonder whether it indicates a more serious genetic disorder. In his book Reardon provides an effective guide to identifying malformations and determining their clinical significance. In the excerpt below Reardon looks at Deep-Set Eyes.
Deep-Set Eyes (more…)
Share This











Nice and clean, acrylic? Ink wash?
Thanks Tim! A bit of both actually.
And a slight bit of pencil work.
*Hahaha* Love the hairstyles going on here. Early Clinton era?