Following on from this year’s Clinical Placement Competition, asking medical students “What does being a doctor mean to you?” – we are hoping to broaden our understanding of the medical profession, and appreciate exactly what being a doctor means in practice. What stories of highlights, difficulties, and uncensored advice can current doctors pass on, and how can we help those starting out?
The post What does being a doctor mean to you? appeared first on OUPblog.
Following on from this year’s Clinical Placement Competition, asking medical students “What does being a doctor mean to you?” – we are hoping to broaden our understanding of the medical profession, and appreciate exactly what being a doctor means in practice. What stories of highlights, difficulties, and uncensored advice can current doctors pass on, and how can we help those starting out?
The post What does being a doctor mean to you? appeared first on OUPblog.
By Rowan Hillson
The first time I increased a patient’s insulin dose I lay awake all night worrying that his blood sugar might fall too low. I was a house officer, and insulin was scary! The patient slept well and safely.
Diabetes is common, chronic and complicated. A recent nationwide audit of 12,191 people with diabetes in 206 English acute hospitals found that 15% of beds were occupied by people with diabetes. Worryingly, 37% of these patients experienced at least one error with their diabetes medications (the full results can be read here).
The National Patient Safety Agency (NPSA) has had over 16,000 reports of insulin incidents. In 2010 the NPSA issued an alert requiring action for all health care professionals to improve prescribing and administration of insulin, which was linked to a “Safe use of insulin” e-learning course.
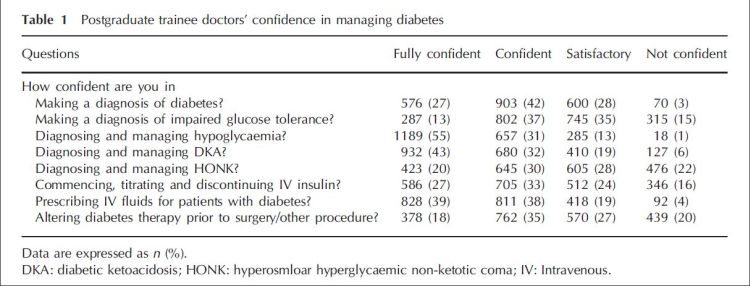
I trained over 30 years ago. Are junior doctors more confident now? Apparently not. A study of 2149 junior doctors by George et al provides worrying evidence that UK trainees lack confidence in managing diabetes. Just 27% were fully confident in diagnosing diabetes, 55% in diagnosing and managing dangerous low glucose and 27% in managing intravenous insulin. Regarding management of diabetes, 24% of respondents would “not often, rarely or never” take the initiative to improve diabetes control. 43% would not adjust insulin in patients with poor glucose control.
Confidence is a combination of knowing what to do and believing you can do it. Experience helps. Also, we all need to know what we don’t know and when to ask for help. An unconfident doctor may make the patient anxious. Galen believed that in the 2nd Century: “Confidence and hope do more good than physic”.
Trainee doctors receive varying amounts of diabetes training and variable supervised experience of looking after people with diabetes. With too little training, trainees may rightly be worried about managing diabetes. Inadequate care of people with diabetes in hospital could worsen virtually every clinical outcome regardless of the main reason for admission. It also worsens patient experience. Diabetes is a common, potentially dangerous but eminently treatable condition. All units in all hospitals should have access to a specialist diabetes team. And trainee doctors should have training and support in diabetes management until they each feel confident in looking after people with diabetes under their care.
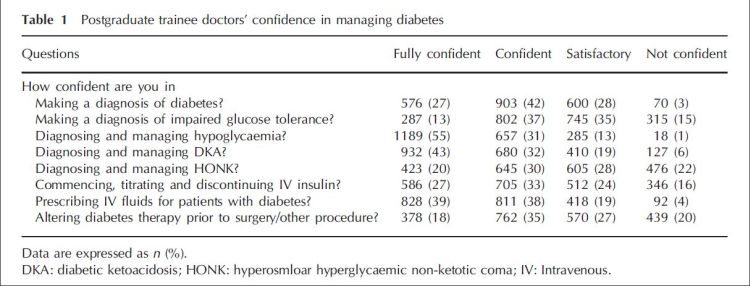
Table from the paper ‘Lack of confidence among trainee doctors in the management of diabetes: the Trainees Own Perception of Delivery of Care (TOPDOC) Diabetes Study’, QJM: An International Medical Journal, Advanced Access, 21 April 2011
Read on for an excerpt from Dr Hillson’s commentary ’Diabetes – big problem, little confidence’, which is published in QJM: An International Journal of Medicine, Advanced Access, 21 April 2011. You can read the
0 Comments on Diabetes: big problem, little confidence as of 1/1/1900