new posts in all blogs
Viewing: Blog Posts Tagged with: ageing, Most Recent at Top [Help]
Results 1 - 7 of 7
How to use this Page
You are viewing the most recent posts tagged with the words: ageing in the JacketFlap blog reader. What is a tag? Think of a tag as a keyword or category label. Tags can both help you find posts on JacketFlap.com as well as provide an easy way for you to "remember" and classify posts for later recall. Try adding a tag yourself by clicking "Add a tag" below a post's header. Scroll down through the list of Recent Posts in the left column and click on a post title that sounds interesting. You can view all posts from a specific blog by clicking the Blog name in the right column, or you can click a 'More Posts from this Blog' link in any individual post.

By: Caroline Ariail,
on 9/13/2015
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
volunteer,
Social Sciences,
*Featured,
ageing,
Health & Medicine,
The Gerontologist,
Gerontology,
National Grandparents Day,
Gerontological Society of America,
Deborah Carr,
Grandparenthood,
Marian McQuade,
Sociology,
Journals,
grandparents,
Grandparent,
Jimmy Carter,
Add a tag
On Sunday September 13, the United States will celebrate National Grandparents’ Day. This annual holiday, held on the first Sunday after Labor Day, celebrates our grandmothers and grandfathers. Marian McQuade, grandmother to 43 and great-grandmother of 15, is widely credited with founding the holiday.
The post Grandparents’ Day: A reading list appeared first on OUPblog.

By:
[email protected],
on 8/20/2015
Blog:
Perpetually Adolescent
(
Login to Add to MyJacketFlap)
JacketFlap tags:
World Dementia Month,
Book News,
picture book,
Author Interviews,
Kayleen West,
elderly,
Shortlist,
Alzheimer's,
Andrew McLean,
dementia,
New Book Releases,
Ford Street Publishing,
Working Title Press,
Aaron Pocock,
Wombat Books,
ageing,
Karen Tyrrell,
Book Reviews - Childrens and Young Adult,
Debra Tidball,
Leigh Hedstrom,
When I see Grandma,
Speech Pathology Australia,
Ellie Royce,
Lucas and Jack,
Romi Sharp,
Celia and Nonna,
Victoria Lane,
Digital Future Press,
Harry Helps Grandpa Remember,
Anna McNeil,
Do You Remember?,
Kelly O'Gara,
Add a tag
Along with a staunch group of Australian literary professionals, Ellie Royce is a strong advocate for promoting encouragement for families to connect with older generations, share love and facilitate the power of memory. Her latest picture book is one in a line up, not only involved in initiatives to create awareness of ageing people and […]

By: Kirsty,
on 7/31/2014
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
health,
Journals,
Medical Mondays,
*Featured,
ageing,
oxford journals,
social care,
age and ageing,
alarms,
Science & Medicine,
Health & Medicine,
catherine henderson,
elderly social care,
telecare,
telehealth,
sensors,
qaly,
demonstrator,
assistive,
Add a tag
By Catherine Henderson
In these times of budgetary constraints and demographic change, we need to find new ways of supporting people to live longer in their own homes. Telecare has been suggested as a useful way forward. Some examples of this technology, such as pull-cord or pendant alarms, have been around for years, but these ‘first-generation’ products have given way to more extensive and sophisticated systems. ‘Second-generation’ products literally have more bells and whistles – for instance, alarms for carbon monoxide and floods, and sensors that can detect movement in and out of bed. These sensors send alerts to a call-centre operator who can organise a response, perhaps call out a designated key-holder, organise a visit to see if there is a problem, or ring the emergency services. There are even more elaborate systems that continuously monitor a person’s activity using sensors and analyse these ‘lifestyle’ data to identify changes in usual activity patterns, but these systems are not in mainstream use. In contrast to telehealth – where the recipient is actively involved in transmitting and in many cases receiving information – the sensors in telecare do not require the active engagement of participants to transmit data, as this is done automatically in the background.
Take-up of telecare remains below its potential in England. One recent study estimated that some 4.17 million over-50 year olds could potentially use telecare, while only about a quarter of that figure were actually using personal alarms or alerting devices. The Department of Health has similarly suggested that millions of people with social care needs and long term conditions could benefit from telecare and telehealth. To help meet this need, it launched the 3-Million Lives campaign in partnership with industry to promote the scaling-up of telehealth and telecare.

The hope held by government and commissioners in the NHS and local authorities is that these new assistive technologies not only promote independence and improve care quality but also reduce the use of health and social care services. To decide how much funding to allocate to these promising new services, these commissioners need a solid evidence base. In 2008, the Department of Health launched the Whole Systems Demonstrator (WSD) programme in three local authority areas in England engaged in whole-systems redesign to test the impacts of telecare (for people with social care needs) and telehealth (for people with long-term conditions).
The research that accompanied the WSD programme was extensive. It included quantitative studies investigating health and social care service use, mortality, costs, and the effectiveness of these technologies. Parallel qualitative studies explored the experiences of people using telecare and telehealth and their carers. The research also examined the ways in which local managers and frontline professionals were introducing the new technologies.
Some results from these streams of research have been published with more to come. From the quantitative research, three articles were published in Age and Ageing over the past year. Steventon and colleagues report on the use of hospital, primary care and social services, and mortality for all participants in the trial – around 2,600 people – based on routinely collected data. Two papers report the results of the WSD telecare questionnaire study (Hirani, Beynon et al. 2013; Henderson, Knapp et al. 2014). The questionnaire study included participants from the main trial who filled out questionnaires about their psychological outcomes, their quality of life, and their use of health and social care services.
The most recent paper to be published in Age and Ageing is the cost-effectiveness analysis of WSD telecare. Participants used a second-generation package of sensors and alarms that was passively and remotely monitored. On average, about five items of telecare equipment were provided to people in the ‘intervention’ group. The whole telecare package accounted for just under 10% of the estimated total yearly health and social care costs of £8,625 (adjusting for case mix) for these people. This was more costly than the care packages of people in the ‘usual care’ group (£7,610 per year) although the difference was not statistically significant. The extra cost of gaining a quality-adjusted life year (QALY) associated with the telecare intervention was £297,000. This is much higher than the threshold range – £20,000 to£30,000 per QALY – used by the National Institute for Health and Care Excellence (NICE) when judging whether an intervention should be used in the NHS (National Institute for Health and Clinical Excellence 2008). Given these results, we would, therefore, caution against thinking that second-generation telecare is the cure-all solution for providing good quality care to increasing numbers of people with social care needs while containng costs.
As with any research, it is important to understand how to best use the findings. The telecare tested during the pilot period was ‘second generation’, so conclusions from this research cannot be applied, for instance, to existing pendant alarm systems currently in widespread use. And telecare systems have continued to evolve since this research started. Moreover, while the results summarised here relate to the telecare participants and do not cover any potential impacts on family carers, there is some evidence that telecare alleviates carer strain.
These findings inevitably raise further questions. What are the broader experiences of those using telecare? What makes a telecare experience positive? And what detracts from the experience? Who can benefit most from telecare? Some answers will emerge as we look across all the findings from the WSD research programme. We also need to look forward to findings from new research, such as the current trial of telecare for people with dementia and their carers (Leroi, Woolham et al. 2013). The ‘big’ question is not whether we should implement a ‘one-size fits all’ solution to meet the increasing demands on social care but for whom do these new assistive technologies work best and for whom are they most cost-effective response.
Catherine Henderson is a researcher at the London School of Economics. She is one of the authors of the paper ‘Cost-effectiveness of telecare for people with social care needs: the Whole Systems Demonstrator cluster randomised trial’, which is published in the journal Age and Ageing.
Age and Ageing is an international journal publishing refereed original articles and commissioned reviews on geriatric medicine and gerontology. Its range includes research on ageing and clinical, epidemiological, and psychological aspects of later life.
Subscribe to the OUPblog via email or RSS.
Subscribe to only science and medicine articles on the OUPblog via email or RSS.
Image credit: Senior woman on phone. © bbbrrn, via iStockphoto.
The post What are the costs and impacts of telecare for people who need social care? appeared first on OUPblog.


By: Kirsty,
on 7/16/2014
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
mental health,
Journals,
Medical Mondays,
happiness,
satisfaction,
*Featured,
ageing,
oxford journals,
age and ageing,
Science & Medicine,
well being,
Health & Medicine,
claire niedzwiedz,
early old age,
life satisfaction,
world map of happiness,
inequalities,
cresh,
creshnews,
bismarckian,
claire_niedz,
niedzwiedz,
health,
Add a tag
By Claire Niedzwiedz
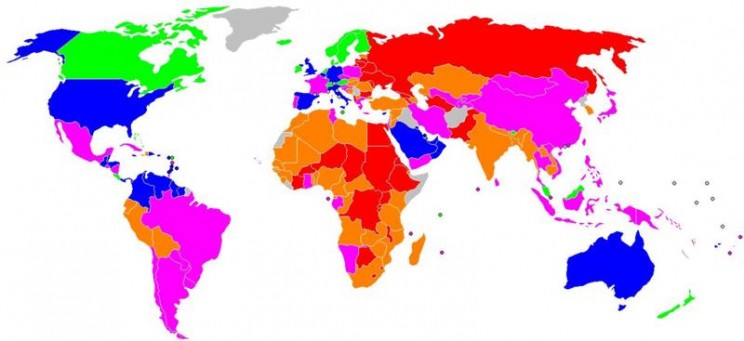
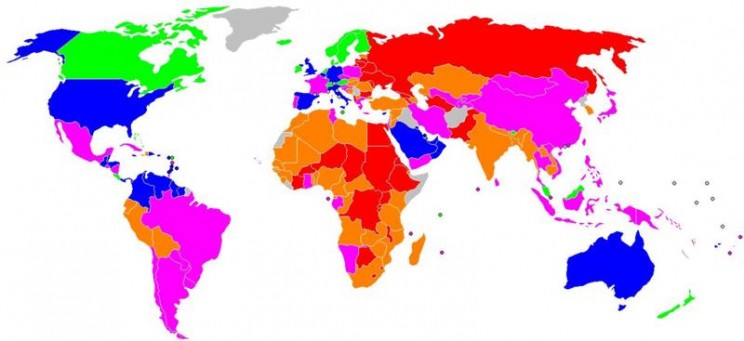
How satisfied are you with your life? The answer is undoubtedly shaped by many factors and one key influence is the country in which you live. Governments across the world are increasingly interested in measuring happiness and well-being to understand how societies are changing, as indicators such as GDP (gross domestic product) do not seem to measure what makes life meaningful. Indeed, some countries, such as Bhutan, have measured national happiness for many years. In the World Map of Happiness below, the countries in green (such as Sweden) have the highest satisfaction. The blue countries are less happy than the green, followed by the pink and orange, and finally the red countries (such as Russia) have the lowest satisfaction. The map conjures up all sorts of interesting questions, like what would the map look like if only older or younger people were included or does happiness vary much within a country?
A U-shaped relationship between age and life satisfaction is often reported, meaning that people are happiest in their 20s and their 60s. But what are the factors that help older people achieve high life satisfaction? Research in this area is particularly important as a result of increasing life expectancy and growth in the proportion of older people. Measuring average well-being is only one side of the story, however. Countries which have high levels of overall life satisfaction may have large inequalities between the richest and poorest in society.
What type of country fosters a more equitable distribution of well-being? This is the focus of our paper recently published in Age and Ageing. We studied the influence of socioeconomic position on life satisfaction in over 17,000 people aged 50 to 75 years old from 13 European countries participating in the Survey of Health, Ageing, and Retirement in Europe (SHARE). To measure socioeconomic position, we used a number of different measures that reflected their position in society at different stages of their life. By looking at their relative position in their own country’s social hierarchy, we created a scale that enabled comparison between countries and across the life course measures. From childhood, we looked at the number of books people reported they had when they were aged 10 years old, a measure of the family’s cultural and economic resources. Education level was used as a measure of early adulthood social position and current wealth was taken as a measure of economic position at the time of the survey. We grouped countries into four categories based on the characteristics of their welfare policy and looked at whether socioeconomic inequalities in life satisfaction varied by the type of welfare state a country fits into.
Intriguingly, we found that Scandinavian (Sweden and Denmark) followed by Bismarckian countries (Germany, Belgium, Switzerland, the Netherlands, Austria, and France) had both higher life satisfaction and narrower differences in well-being between those at the top and bottom of society. Scandinavian countries are traditionally characterised by their high levels of welfare provision, universalism, and the promotion of social equality. Bismarckian countries are characterised by welfare states that maintain existing social divisions in society, in which social security is often related to one’s earnings and administered via the employer. Southern (Greece, Italy, and Spain) and Post-communist (Poland and the Czech Republic) countries, which tend to have less generous welfare states, had lower life satisfaction and larger social inequalities in life satisfaction. The number of books in childhood was a significant predictor of quality of life in early old age in all welfare states, apart from the Scandinavian type, and the relationship was particularly strong among women in the Southern countries. On the whole, however, inequalities in life satisfaction were largest by current wealth across the majority of welfare states.
Our findings have important implications, especially given the welfare policy changes taking place across Europe and the growth in wealth inequalities. It raises questions about how future generations of people are going to experience their early old age. Will average well-being and inequalities between the richest and poorest change as less welfare support is available? What will be the impact of increases in the retirement age? It is clear that these are urgent questions which affect us all and that the policies governments pursue are likely to shape the answers.
Claire Niedzwiedz (@claire_niedz) is a final year doctoral researcher at the University of Glasgow’s Institute of Health and Wellbeing and is part of the Centre for Research on the Environment, Society and Health (CRESH). They tweet at @CRESHnews. She is the author of the paper ‘The association between life course socioeconomic position and life satisfaction in different welfare states: European comparative study of individuals in early old age’, published in the journal Age and Ageing.
Age and Ageing is an international journal publishing refereed original articles and commissioned reviews on geriatric medicine and gerontology. Its range includes research on ageing and clinical, epidemiological, and psychological aspects of later life.
Subscribe to the OUPblog via email or RSS.
Subscribe to only science and medicine articles on the OUPblog via email or RSS.
Image credit: Satisfaction with Life Index Map coloured according to The World Map of Happiness, Adrian White, Analytic Social Psychologist, University of Leicester. Public domain via Wikimedia commons
The post Inequalities in life satisfaction in early old age appeared first on OUPblog.


By: Kirsty,
on 1/21/2013
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
depression in old age,
geriatric depression scale,
siegfried weyerer,
weyerer,
incidence,
siegfried,
functional,
health,
Medical Mondays,
depression,
Psychology,
smoking,
senior citizens,
psychiatry,
old age,
dementia,
epidemiology,
eldery,
Editor's Picks,
*Featured,
ageing,
haas,
oxford journals,
age and ageing,
Science & Medicine,
Health & Medicine,
impairment,
Add a tag
By Siegfried Weyerer
Depression in old age occurs frequently, places a severe burden on patients and relatives, and increases the utilization of medical services and health care costs. Although the association between age and depression has received considerable attention, very little is known about the incidence of depression among those 75 years of age and older. Studies that treat the group 65+ as one entity are often heavily weighted towards the age group 65-75. Therefore, the prediction of depression in the very old is uncertain, since many community-based studies lack adequate samples over the age of 75.
 With the demographic change in the forthcoming decades, more emphasis should be put on epidemiological studies of the older old, since in many countries the increase in this age group will be particularly high. To study the older old is also important, since some crucial risk factors such as bereavement, social isolation, somatic diseases, and functional impairment become more common with increasing age. These factors may exert different effects in the younger old compared to the older old. Knowledge of risk factors is a prerequisite to designing tailored interventions, either to tackle the factors themselves or to define high-risk groups, since depression is treatable in most cases.
With the demographic change in the forthcoming decades, more emphasis should be put on epidemiological studies of the older old, since in many countries the increase in this age group will be particularly high. To study the older old is also important, since some crucial risk factors such as bereavement, social isolation, somatic diseases, and functional impairment become more common with increasing age. These factors may exert different effects in the younger old compared to the older old. Knowledge of risk factors is a prerequisite to designing tailored interventions, either to tackle the factors themselves or to define high-risk groups, since depression is treatable in most cases.
In our recent study, over 3,000 patients recruited by GPs in Germany were assessed by means of structured clinical interviews conducted by trained physicians and psychologists during visits to the participants’ homes. Inclusion criteria for GP patients were an age of 75 years and over, the absence of dementia in the GP’s view, and at least one contact with the GP within the last 12 months. The two follow-up examinations were done, on average, one and a half and then three years after the initial interview.
Depressive symptoms were ascertained using the 15-item version of the Geriatric Depression Scale (GDS). We found that the risk for incident depression was significantly higher for subjects
- 85 years and older
- with mobility impairment and vision impairment
- with mild cognitive impairment and subjective memory impairment
- who were current smokers.
It revealed that the incidence of late-life depression in Germany and other industrialized countries is substantial, and neither educational level, marital status, living situation nor presence of chronic diseases contributed to the incidence of depression. Impairments of mobility and vision are much more likely to cause incidents of depression than individual somatic illnesses such as diabetes mellitus and coronary heart disease. As such, it is vital that more attention is paid to the oldest old, functional impairment, cognitive impairment, and smoking, when designing depression prevention programs.
GP practices offers ample opportunity to treat mental health problems such as depression occurring in relation to physical disability. If functional impairment causes greater likelihood of depression, GPs should focus on encouraging older patients to maintain physical health, whether by changing in personal health habits, advocating exercise, correcting or compensating functional deficits by means of medical and surgical treatments, or encouraging use of walking aids. Additionally, cognitive and memory training could prevent the onset of depressive symptoms, as could smoking cessation. If these steps are taken, the burden of old age depression could be significantly reduced.
Siegfried Weyerer is professor of epidemiology at the Central Institute of Mental Health in Mannheim, Germany. He has conducted several national and international studies on the epidemiology of dementia, depression and substance use disorders at different care levels. He is also an expert in health/nursing services research. He is one of the authors of the paper ‘Incidence and predictors of depression in non-demented primary care attenders aged 75 years and older: results from a 3-year follow-up study’, which appears in the journal Age and Ageing. You can read the paper in full here.
Age and Ageing is an international journal publishing refereed original articles and commissioned reviews on geriatric medicine and gerontology. Its range includes research on ageing and clinical, epidemiological, and psychological aspects of later life.
Subscribe to the OUPblog via email or RSS.
Subscribe to only health and medicine articles on the OUPblog via email or RSS.
Image credit: Grief. Photo by Anne de Haas, iStockPhoto.
The post Depression in old age appeared first on OUPblog.


By: Nicola,
on 12/17/2012
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
cardiovascular risk factors,
cognitive decline,
dr alex dregan,
framingham,
older adults,
population study,
risk factors,
vascular disease,
vascular,
cardiovascular,
antihypertensive,
dregan,
smoking,
forgetfulness,
stroke,
public health,
high blood pressure,
cognitive,
cholesterol,
bmi,
epidemiology,
*Featured,
ageing,
oxford journals,
age and ageing,
Science & Medicine,
Health & Medicine,
forgetful,
Add a tag
By Dr Alex Dregan
Do vascular risk factors such as high blood pressure and smoking make us forgetful?
As our bodies start to show the signs of ageing, our brain is naturally ageing too. But some older people can become forgetful and have trouble remembering common words or organising daily activities more than others. There are few proven interventions to prevent this kind of cognitive decline in older adults, although treating modifiable risk factors for vascular disease and stroke, such as cholesterol and body mass index (BMI), has been suggested as a promising approach to preventing or delaying cognitive impairment for a growing UK population of older adults. So is there a link between high blood pressure and forgetfulness?
Despite much recent interest, studies to date have reported inconsistent relationships between blood pressure and cognitive functioning. Evidence suggests that people diagnosed with high blood pressure levels tend to perform more poorly on most domains of cognitive functioning, including memory, learning, attention, and reasoning. However, clinical trials have so far failed to demonstrate that antihypertensive drugs used to lower or control high blood pressure levels are effective in preventing cognitive decline in older adults. This inconsistent evidence poses a challenge when developing recommendations for the prevention of cognitive ageing.
Cognitive ageing, such as symptoms of forgetfulness, is increasingly seen as the result of the joint effect of several vascular disease risk factors, including high blood pressure, BMI, cholesterol levels, and smoking. However, the combined influence of these on cognitive decline is less commonly explored among older adults at increased risk of both cardiovascular disease and cognitive decline.
In a recent paper, we looked at Framingham stroke and cardiovascular risk scores (a measure used to assess an individual’s probability of developing stroke or cardiovascular disease over a 10-years period) and investigated their association with cognitive decline in older adults. The study included over 8,000 adults aged 50+ living in private households in England. Participants with the highest risk of future stroke or cardiovascular events, based on their risk factors values, were found to perform more poorly on tests of memory and executive functioning after a four year period. This adds weight to the theory that the combined effects of risk factors for vascular disease and stroke may be associated with more rapid cognitive decline in older adults. In other words, those at greater risk of cardiovascular problems were likely to experience a more rapid onset of symptoms associated with cognitive decline, such as forgetfulness.
We believe that these findings support the need for a multifaceted approach when seeking to prevent cognitive decline. The main implication of this is the need for addressing the combined effect of multiple risk factors, including lowering high blood pressure and high cholesterol levels, weight loss, and stopping smoking. Thus, healthcare professionals should encourage older people to adopt healthy lifestyles that would include stopping smoking and increased exercise (as well as improved diet not investigated here) and taking prescribed medicines aimed at controlling high blood pressure and high cholesterol levels. Such recommendations could potentially prevent or delay future declining memory or reasoning capacities in older adults, particularly those in higher risk groups.
The results also suggest that a harmful effect of high blood pressure on memory or reasoning abilities may develop over a prolonged period of time. This may be one reason why short-term trials have failed to show a consistent benefit from antihypertensive treatment on cognitive decline. For instance, since the negative impact of high blood pressure on memory or reasoning abilities takes place over a prolonged period of time, short-term treatment may not be sufficient to reverse or delay its adverse influence. Therefore, we would expect that any potential cognitive benefits from lowering blood pressure may only be observed over substantial periods of time.
These new results suggest that attention to the combined effects of multiple vascular risk factors may hold some promise as a strategy to prevent cognitive decline in older adults.
Dr Alex Dregan is a Lecturer in Translational Epidemiology within the NIHR Biomedical Research Centre at the Guy’s and St Thomas’ NHS Trust and King’s College London. He trained in Public health at the Institute of Education, University of London. His research interests are in translational epidemiology research as applied to public health. He is co-author of the paper Cardiovascular risk factors and cognitive decline in adults aged 50 and over: a population-based cohort study for the Age and Ageing journal, and this has been made freely available for a limited time.
Age and Ageing is an international journal publishing refereed original articles and commissioned reviews on geriatric medicine and gerontology. Its range includes research on ageing and clinical, epidemiological, and psychological aspects of later life.
Subscribe to the OUPblog via email or RSS.
Subscribe to only health and medicines articles on the OUPblog via email or RSS.
The post The ageing brain appeared first on OUPblog.


By: Nicola,
on 12/12/2011
Blog:
OUPblog
(
Login to Add to MyJacketFlap)
JacketFlap tags:
health,
elderly,
diabetes,
disability,
mobility,
geriatric,
*Featured,
ageing,
oxford journals,
age and ageing,
diabetic,
Science & Medicine,
Health & Medicine,
evelien pijpers,
older persons,
recurrent falls,
evelien,
pijpers,
recurrent,
maastricht,
Add a tag
Whilst browsing the Oxford journal Age and Ageing last week, I came across a paper focusing on diabetes in the elderly. Interestingly, it noted that men and women with diabetes aged 65 or over are one and half times more likely to have recurrent falls than people in the same age bracket without diabetes. Having two sets of grandparents in their seventies, one pair with diabetes and one without, I wanted to know about this correlation between diabetes and falling, and how it might apply to them. Here, I speak with Ms. Evelien Pijpers (EP), author of this paper, to learn more. – Nicola (NB)
NB: Your recent paper says that in a three-year study of 1145 Dutch participants aged 65 and over, you discovered an increased risk of recurrent falls associated with diabetes. Can you explain why those with diabetes are more likely to have a fall?
EP: We examined a number of possible contributing factors which led to this increased likelihood of recurrent falls, yet we can only explain about half of the increased risk faced by older patients with diabetes.
The factors which we did link with the increased risk of recurrent falling in patients with diabetes included the use of four or more medications; higher levels of chronic pain, mostly experienced in the muscles and bones; poorer self-perceived health; lower physical activity, grip strength and sense of balance, combined with greater limitations in the performance of daily activities such as bathing and dressing; and more significant problems with cognitive impairment.
Fortunately for the patients, we didn’t record enough major injuries or fractures over the three-year study period to be able to track any correlation between diabetes and fracture risk in older people.
NB: What are the consequences of recurrent falling?
EP: As a geriatrician, I see a lot of mobility problems in older patients. They are present in older people in the accident and emergency department, the hospital wards, and the care and nursing homes. When I visit my older patients at home, it is both the mobility difficulties and the fear of falling which stop them from walking to the shops or strolling through the cobblestone streets of Maastricht.
My older patients with diabetes seem to be especially prone to fall and injure themselves. Even if they avoid lasting injury, I find that afterwards they try and avoid situations in which they could fall again. This unfortunately limits their social contact and the number of physical activities they are willing to undertake, and as such their physical condition declines, sometimes to the point where disability and loss of independence are inevitable. For those with diabetes who are more likely to fall, it is more likely that they will face this quandary.
NB: So what could be done to prevent the increased fall risk in older persons with diabetes?
EP: To improve the quality of life of this growing group of older patients with diabetes, it is important to keep them physically and mentally active, mobile, and able to avoid falls and injuries. Therefore even though we cannot yet account for the entirety of the increased risk of falling, it is possible to address fall risk factors we now know about. A medication review can help, as can muscle training and activities to improve balance – which in turn may even improve pain induced by osteoarthritis. Improving mobility helps individuals to perform everyday activities, and it is easier to feel positive about your health if you are able to maintain independence. It is important that we teach older patients how to fall with the least risk of injury, and how to pick yourself up (both physically and mentally) when you have fallen without losing confidence. As such, physicians should be in the practice of counselling all elderly diabetic patients about active lifestyles and the importance of mobi