How is new medical technology changing the treatment of pain? How are views of chronic pain changing? Could England have made it to the World Cup final this Sunday if some players hadn’t gone into pain medicine? We spoke to Mark Johnson, Professor of Pain and Analgesia at Leeds Metropolitan University, about his research into pain medicine, the future of the field, and most importantly, how he almost considered becoming a professional footballer.
When did you first become interested in pain science?
I first become interested in pain science in 1984 whilst studying for a BSc in physiology at the University of Leeds. I have always been fascinated with self-awareness and the physiology of sensations and in the final year of my BSc I was lucky enough to investigate how the brain modulates nerve impulses arising in tissue damage. I remember the thrill of discovering that stimulating neurons in the Periaqueductal Grey of the brainstem stopped activity of ‘pain’ neurons in the spinal cord. This provided indirect evidence that the sensation of pain could be modified by the brain. Nowadays patients with severe intractable pain may receive deep brain stimulation where fine electrodes are implanted into the Periaqueductal Grey to administer weak pulsed electrical currents to reduce the patient’s pain.
Over the years my interests diversified and I currently lead a team of researchers undertaking programmes of research on:
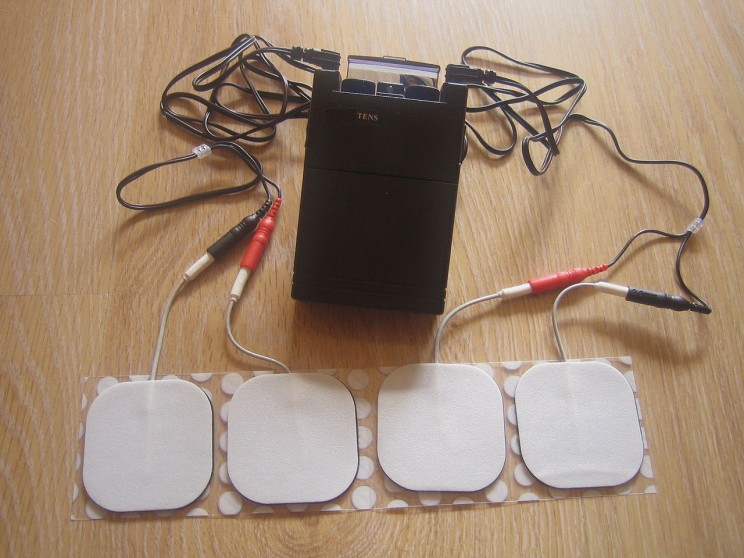
- Factors influencing response to electrophysical agents including, TENS (Transcutaneous Electrical Nerve Stimulation), low-level laser therapy, acupuncture, massage, manipulation, and mobilization
- Factors influencing pain sensitivity response, including sex/gender, ethnicity, and obesity
- The epidemiology of pain in developing countries
- Pain, motor imagery, and perceptual embodiment
- Patient experiences of pain
For me the attraction of researching the science of pain is that it is multidisciplinary. Our research involves physics, chemistry, genetics, physiology, pharmacology, medicine, psychology, sociology, and spirituality. What a mix!
What do you think has been the biggest change in pain medicine in the past 10 years?
It really depends on which discipline within pain medicine you are studying. I am particularly interested in the increased use of high tech treatments such as electrical stimulators that can be implanted into various parts of the body including the spinal cord and brain to relieve severe intractable pain. Yet I am also interested in low tech treatments such as using mirrors to create visual illusions to reduce pain, such as mirror box therapy. Over the last decade insights into the genetics and physiology of pain have informed clinical practice. Routine screening for neuropathic pain, which is managed using different medication to non-neuropathic pain has vastly improved care for these patients. The understanding that the body may exist in a persistent pain state despite the absence of tissue damage has altered the way we manage chronic pain and made us realize that the pain system itself may became dysfunctional. In other words pain may exist as a disease entity in its own right. A programme of research conducted by our team on genetic profiling codeine non-responders will help to tailor pain treatment more effectively for individuals.
![By National Cancer Institute [Public domain], via Wikimedia Commons](http://blog.oup.com/wp-content/uploads/2014/06/Doctor_consults_with_patient_4.jpg)
What is the most pressing or controversial issue in your field right now?
Perhaps the most pressing issue is the need to address the burden of chronic pain. Our research has shown that the prevalence of chronic pain worldwide is over 25% dwarfing many well-known conditions such as heart disease and diabetes. There is a debate about the best way to deal with this problem as medical and psychosocial models of care are only partially effective. Generally, there has been a shift to psychosocial models of care for many types of chronic pain in recent years. I believe far more attention needs to be given to environmental factors that contribute to chronic pain, especially in modern societies where there is a lack of physical activity due to sedentary lifestyles.
Why did you decide to write a book about this topic?
I have been researching into TENS since 1987 and during that time there has been an on-going debate about whether TENS is clinically effective (i.e. superior to placebo). There is a vast research literature on TENS with over 500 clinical studies but findings have been inconsistent. This has resulted in the National Institute of Health and Care Excellence (NICE) recommending TENS for some painful conditions but not for others. Practitioners and patients are confused about whether they should use TENS and if they do how best to administer it. I wrote the book to provide comprehensive coverage of research findings to inform safe and appropriate TENS technique. I also wanted to synthesize evidence about effectiveness and offer solutions to overcome the challenges faced when designing good clinical studies. The last book on TENS was published over 15 years ago.
How might your current research have an impact on the wider world?
The research on TENS conducted by our team over a 15 year period has furthered our understanding of how best to administer TENS. Importantly, we have demonstrated that patients and practitioners are satisfied with TENS and they can use it in combination with other pain treatments helping to reduce medication, which may have unpleasant side effects. TENS is relatively inexpensive, can be self-administered by patients as needed and can be purchased by patients without prescription. We have found that TENS is used widely in resource rich countries but less so in resource-limited countries. Recently, we published the findings of some surveys that found that TENS was not being used to its full potential in India and Sri Lanka so we are looking at ways of trying to integrate TENS into pain management strategies in these countries.
Which person has been most influential to the way you do your job?
That’s a difficult question. The most influential people would be my PhD supervisors, Professor John Thompson and Professor Heather Ashton. They taught me the importance of academic rigor by being diligent in the design, execution, analysis, and dissemination of research investigations. They instilled in me the importance of publishing research findings — it is pointless doing research if nobody finds out about it. I guess the author Scott Adams must also get a mention because his book “The Dilbert Principle” helped me to survive the day to day nonsense that goes on at the workplace!
What advice would you give to someone wanting to specialize in your field?
Be inquisitive and reflective. Be open minded to allow your perspective to be changed but not so open minded that your brain falls out and you start to act on hearsay rather than evidence. Be humble in your views as you will be wrong from time to time. Most of all be passionate and have fun.
What do you see as being the future of research in your field in the next decade?
Research into the genetics of pain and the genetics of treatment response will enable therapies to be tailored more precisely to individuals. Our investigations on the prevalence and genetic profile of codeine non-responders in chronic pain patients has a long term goal of developing a simple screening test so practitioners will know whether a patients is likely to respond to analgesic medication at the point of care. Recent technological developments in multi array electrodes for TENS will provide more precise and effective stimulation.
If you weren’t working in pain medicine, what would you be doing?
I love writing, teaching, and finding things out so I couldn’t imagine myself working outside of academia. If I were not researching in pain science then I would like to work in the field of neuropsychology on self-awareness. If I weren’t an academic, I would probably have ended up as a sports coach. I have played competitive sports all of my life and enjoy helping others reach their full potential. As a teenager I played soccer at Wallsend Boys Club, famous for fostering Peter Beardsley, Steve Bruce, Alan Shearer, and Michael Carrick. I briefly contemplated becoming a professional soccer player but I much preferred science . . . and I wasn’t a good enough footballer to make the big time. For the last 15 years I have cycle raced, and have developed a chronic back pain problem as a consequence. I could not see myself as professional racing cyclist because it involves far too much suffering — I prefer my pain to be intellectual rather than physical.
Mark I. Johnson is Professor of Pain and Analgesia at Leeds Metropolitan University. He is the author of Transcutaneous Electrical Nerve Stimulation (TENS): Research to support clinical practice. You can find Leeds Metropolitan University’s Pain Science department on Facebook.
Subscribe to the OUPblog via email or RSS.
Subscribe to only health and medicine articles on the OUPblog via email or RSS.
Images: (1) Doctor consults with patient by National Cancer Institute. Public domain via Wikimedia Commons. (2) TENS (Transcutaneous Electrical Nerve Stimulator) by Yeza. CC-BY-SA-3.0 via Wikimedia Commons via Wikimedia Commons.
The post Catching up with Mark Johnson, pain science specialist appeared first on OUPblog.




